On Jan. 20, Australian psychiatrist Dr. Ted Cassidy posted on LinkedIn that he made history by becoming the first doctor in the modern era to write a prescription for a psychedelic substance.
If true, it’s a major milestone for the nascent field of psychedelic medicine.
While Psychedelic Medical News could not verify Cassidy’s claim, Mind Medicine Australia, a nonprofit research group focused on psychedelic therapy, issued a statement on Jan. 19 stating that Cassidy and Dr. Eli Kotler administered the first psychedelic treatment sessions in a clinical setting in 50 years.

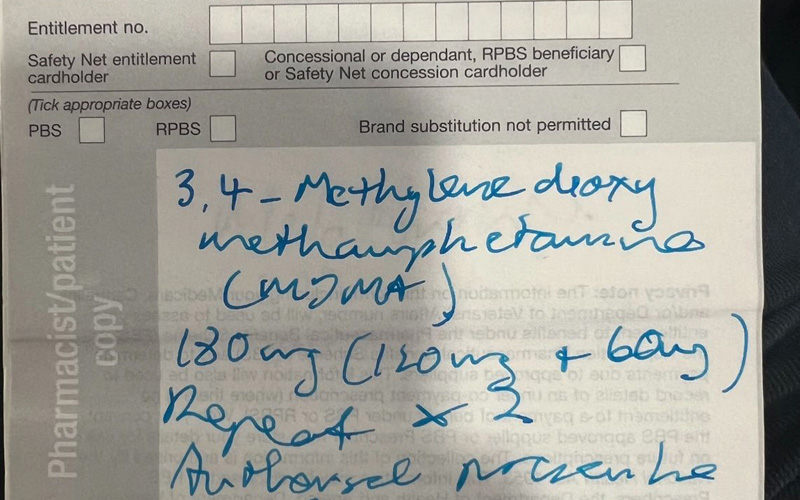
Along with a photo of the MDMA prescription that he wrote, Cassidy said:
“Today’s treatment is the world’s first psychedelic-assisted therapy (PAT) treatment ever given outside of research and compassionate use protocols. Monarch Mental Health Group developed this program over the last year building on Monarch’s record of innovation in outpatient mental health treatments over the last 10 years. I am proud to have been part of the team at Monarch that has made this the first clinical Psychedelic program available to patients in the world. I am proud that Australia has taken world leadership in translating psychedelic research into clinical reality.”
In July 2023, Australia became the first country to approve MDMA and psilocybin for treatment-resistant depression and post-traumatic stress disorder.
PMN Editorial Director John Scott spoke with Cassidy over Zoom just days after he finished administering his first psychedelic-assisted therapy treatment. The following is an edited version of that conversation.
JS: Can you tell me a little bit about your organization and background?
TC: Monarch Mental Health Group is an Australian-based mental-health organization that for the last seven or eight years has been involved in next-step interventional outpatient treatments for mental health. And basically, we’re interested in the new stuff. It started off when I got involved in magnetic-stimulation therapy, which is an outpatient treatment, and we’re now the largest provider of that in Australia. And we work with a number of other treatments. We’ve been offering esketamine and oral ketamine, transcranial direct-current stimulation devices. We’re the next step when you haven’t had a good response to all the standard sort of medications and psychotherapy.
We got interested in psychedelics from a research point of view when the government in Australia began offering funding and prioritized research in psychedelics. And then, by complete surprise, earlier last year the government essentially legalized psychedelics for use in people who have either treatment-resistant depression or chronic treatment-resistant post-traumatic stress disorder. [Australia] was the first in world. We then basically just started pedaling hard to get a clinical program going. We were in a really good position to do that because we already had research trials going, and we had staff who were familiar with psychedelics. And then, as a result, our first patient was treated about a week-and-a-half ago on Jan. 19.
JS: Can you tell me a little bit about the protocol you followed and how the first treatment went?
TC: It was a fairly conventional course of MDMA-assisted psychotherapy. It was very much based on the MAPS protocols from the U.S., which just had their Phase 3 trials. We had a very similar approach. We assessed a patient, someone with chronic PTSD, who had a complicated case of PTSD based on a traumatic childhood and adolescent experiences. We then enrolled the patient in the clinical program. They had three preparation sessions conducted jointly with myself as the psychiatrist and Monica Schweickle as the clinical psychologist. Then we all got together for the MDMA therapy session, and during that session she had an initial dose of 120 milligrams and a top-up dose of 60 milligrams to get to a total dose of 180 milligrams, and the session was for about eight to 10 hours.
I’ve never been involved in a psychedelic-assisted therapy session before, and surprisingly it was almost exactly the way everyone describes it in the books. It was really, to be honest, one of the more straightforward psychotherapy sessions I’ve ever been involved in. It was really quite easy. It was easier because the patient was able to do all the stuff that you’re supposed to do with MDMA. They were able to just think clearly, speak rationally. The kind of fear centers that normally prevent discussions were kind of switched off temporarily. It was really amazing just to see the patient talk about stuff in a really open, logical way, and then manage some of those feelings and look at strategies about ways to deal with that.
With traditional psychotherapy for PTSD, you might spend years before you can even have that opportunity. To have a single disruption on those times to be able to do it almost on queue was incredible. We saw the patient the following day for their first integration session. And I think it is fair to say that when people come back 12 hours afterwards, and the MDMA is no longer active in their system, I think that’s a really important time because often they’re reflecting, and they’re thinking, ‘Oh my god, did I really talk about all this stuff? How do I feel about it?’ And so, we’re very aware of that and able to provide the necessary reassurance and label the whole experience as a really positive experience rather than something to feel embarrassed about. And we’ve been following up with this patient since then. We’re only partway through the program. She’s had one dosing so far, and she has another coming in about two weeks, and then there’ll be another one three weeks after that.
JS: You mentioned that the session took about eight to 10 hours. Can you describe what happened during that period?
TC: There was a bit of prep and admin stuff at the beginning, and then we gave the dose. She just kind of sat quietly for about an hour, hour-and-a-half. We gave the second dose and monitored her blood pressure. At one point , she sat up, and had like a light-bulb moment. The next four or five hours was a really rich period of a lot of talking, a lot of discussion about things. I could see how in a recreational environment the opportunity would be wasted because really there wasn’t a lot of focus or structure initially. And we used a lot of grounding exercises and deep breathing and a range of strategies to slow down the process, so that she had time to internally work through things before she actually started talking about them.
To me, it felt like we got further in that one day than we would normally get in a year’s worth of therapy. I’ve had patients with PTSD that I’ve been talking to for years, and we don’t get anywhere. And I felt like within that one session with a patient that I’d met three or four times before, over a period of maybe six to eight weeks of preparation, that we were really able to dive into the problem areas in a way that was surprising and simple.
JS: What do you look for when you’re screening patients to ensure safety?
TC: Well, people with comorbid mental illness, a presence of mania or presence of schizophrenia, people with heart conditions based on hypertension is a problem. That’s because MDMA tends to elevate blood pressure during the treatment regimen. That was quite notable, even with this patient, that her systolic and diastolic both increased about 10 to 15 millimeters of mercury baseline, and her heart rate went up about 10 to 15 beats per minute. So nothing in the dangerous range. But during the peak effect, that sort of four to five hours in the middle of treatment, there was a significant elevation of blood pressure and pulse rate over baseline. People that are very underweight or very overweight, we have some concerns about, partly because of the dosing. If you’re on a serotonin increasing drug – and this applies either to MDMA or psilocybin – that’s a big problem, so you need to get patients off their antidepressants.
JS: Have you begun working with psilocybin as well?
TC: Yeah, we have. And we’ll probably have our first psilocybin patient sometime in the next month or two.
JS: And is the process similar with that?
TC: Very similar in terms of the prep and the protocol. The big difference, which I’m anticipating will be in the session, is that MDMA is a very active verbal session, whereas the psilocybin session is much more internal for the patient. So it’s a much more a quiet, non-breakthrough-style session. And a lot of the work comes in the integration where people sort of reflect upon the experience they had during that psilocybin experience and make the various connections.
JS: So what do you see in the coming years for psychedelic therapy? What’s next?
TC: I think this is really the beginning of the treatments, and I think there are some real disadvantages to the way it’s been done at the moment. I mean, it’s incredibly labor-intensive, which makes it expensive and it makes it difficult to access. So in these early stages, it’s really a third-line treatment for patients who’ve really tried everything else simply because of the cost and the inconvenience and the lack of availability. I think over the next couple of years we’re going to see more and more clinical programs such as ours taking on different aspects of the therapy, and I think that’ll be good for patients. They’ll have some diversity. I think what we do need to think about is how we can do these things more efficiently.
At the moment, we’ve got a psychiatrist and a clinical psychologist delivering the therapy, and I’d like to see a point where we could have a psychedelic therapist – perhaps someone who isn’t a psychiatrist or psychologist – working with maybe a psychologist delivering the therapy. That would certainly bring down the cost and improve the availability for the patients. We’re looking at things like group-based therapy. Again, this is very early stages, but I think that would certainly dramatically reduce cost. Certainly, my experience of that single therapy session was that I don’t think we could have achieved what we achieved if we’d had it in a group session. So, in theory, I like the idea of groups because it’s cost-effective, but I’m not certain yet whether it will ever be practical. Maybe more so with psilocybin, depending on if it is a much more internal experience.
JS: Can you give me an idea of what the sessions cost?
TC: The U.S. dollar cost is probably around $15,000 for a course of three dosing sessions, plus all the prep and integration. But we are seeing at this early stage some interest from our veteran services in terms of supporting veterans. And they’ve been one of the big advocacy groups. The real promise of these treatments is you’re aiming to get people 100% well. We’ll see how that pans out in time. I’m not overpromising or even setting my expectations too high, but certainly when you’re talking about psychedelic-assisted therapy, it’s about a step change rather than just small increments.